If you check out the CDC’s release of data concerning STIs, you’ll notice that cases of chlamydia have been declining- but it might be too soon to celebrate this news. Unlike other STIs, like gonorrhea, which presents with painful, irritating symptoms that prompt people to seek treatment, chlamydia is notorious for causing “silent infections” (aka being asymptomatic), so many people don’t know they have it until they get tested. Concomitantly, general screenings have decreased, especially during the peak of COVID-19, so it poses the question- did cases of chlamydia really decline, or does it just seem like they did because screenings are down, and infections aren’t being detected?
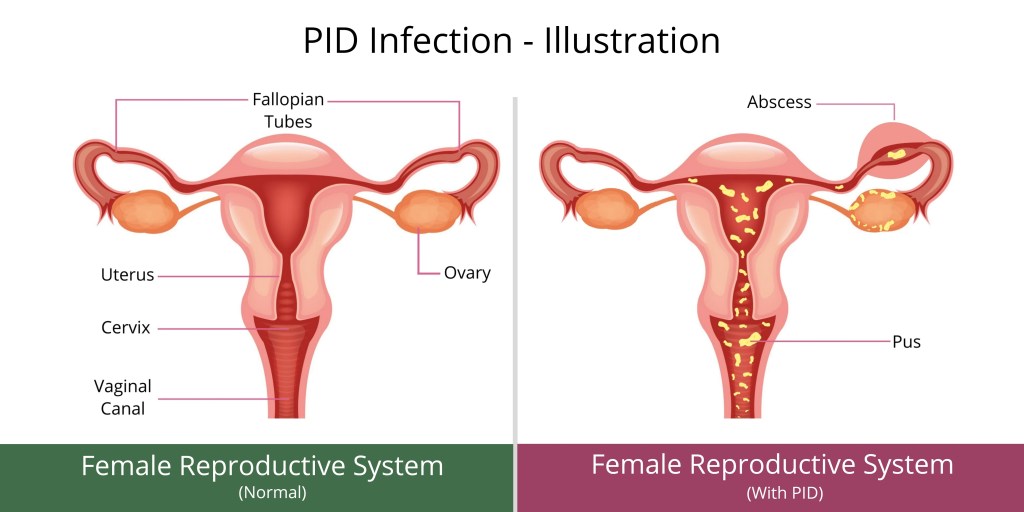
Chlamydia can lead to PID, otherwise known as pelvic inflammatory disease, which poses a huge threat to female fertility since it can lead to infertility. PID can cause many complications, including scar tissue formation which can block the Fallopian tubes, ectopic pregnancies, and chronic pelvic/abdominal pain. Moreover, if a woman is pregnant and has chlamydia, she is at higher risk for preterm delivery, and can spread the infection to her baby during delivery, which can cause the baby to suffer from eye infections or pneumonia. Men seldom have long-term complications from the infection, however, in rare cases it can affect the tubes attached to the testicles, which can result in infertility as well.
It is strongly recommended that sexually active women get tested for chlamydia every year if:
- Younger than 25 years old.
- 25 years and older with risk factors, such as new or multiple sex partners, or a sex partner who has a sexually transmitted infection.
It’s important that routine screening be implemented in primary care practices to ensure the wellbeing of their patients’ reproductive health. One of the beneficial things that resulted from COVID-19 was the availability of testing. Some practices now perform appointments via Telehealth and allow patients to drop off samples, facilitating the whole process. Additionally, at-home rapid tests and test kits have become more common. Today, you can purchase a basic kit that tests for chlamydia, gonorrhea and trichomoniasis. You can even find a test kit on Amazon, like LetsGetChecked or Everlywell for example. and get it delivered the next day. There are several tests, even ones that can be tailored to your gender, or specific concerns. It’s important to note that the best place to get tested is a clinic, because not all kits may be FDA approved.
The take home message is this: even if patients are asymptomatic now, some STIs can have long-term fertility consequences, and it’s essential you stay up to date on your check-ups and screenings.








